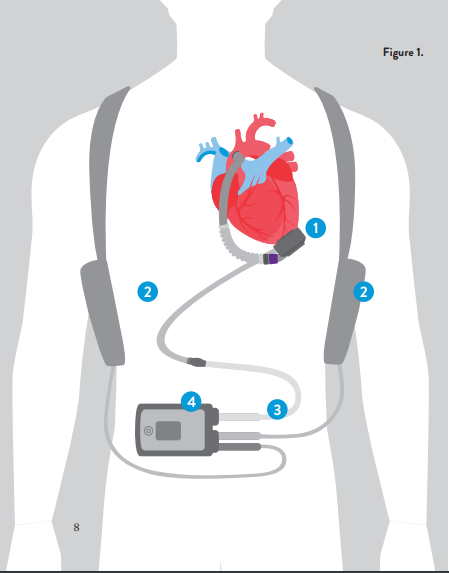
LVAD treatment is for patients who have been diagnosed with advanced heart failure, a condition in which the heart cannot pump enough blood to meet the body’s needs. Click here to learn about heart failure.
Patients who have advanced heart failure have debilitating symptoms. They often have multiple hospital visits each year, experience lower blood pressure and defibrillator discharges. They may also have a poor appetite, weight changes and fatigue and find themselves unable to take heart medication because of dizziness. These patients have a poor prognosis, in some cases between 45 and 75 percent one-year mortality without advanced therapy. Thus, the mortality rate can be worse than some cancers.
LVAD it is used for patients who need short- or long-term mechanical circulatory support and for whom transplant is not an option. This technology is not suitable for all patients with end-stage heart failure, for example, those who have infections or conditions like liver disease, lung disease, kidney failure, allergies to anticoagulation products, as well as other complicating factors.